Weight-loss medications such as Wegovy are designed for extended periods of use, but some patients are interested in discontinuing them
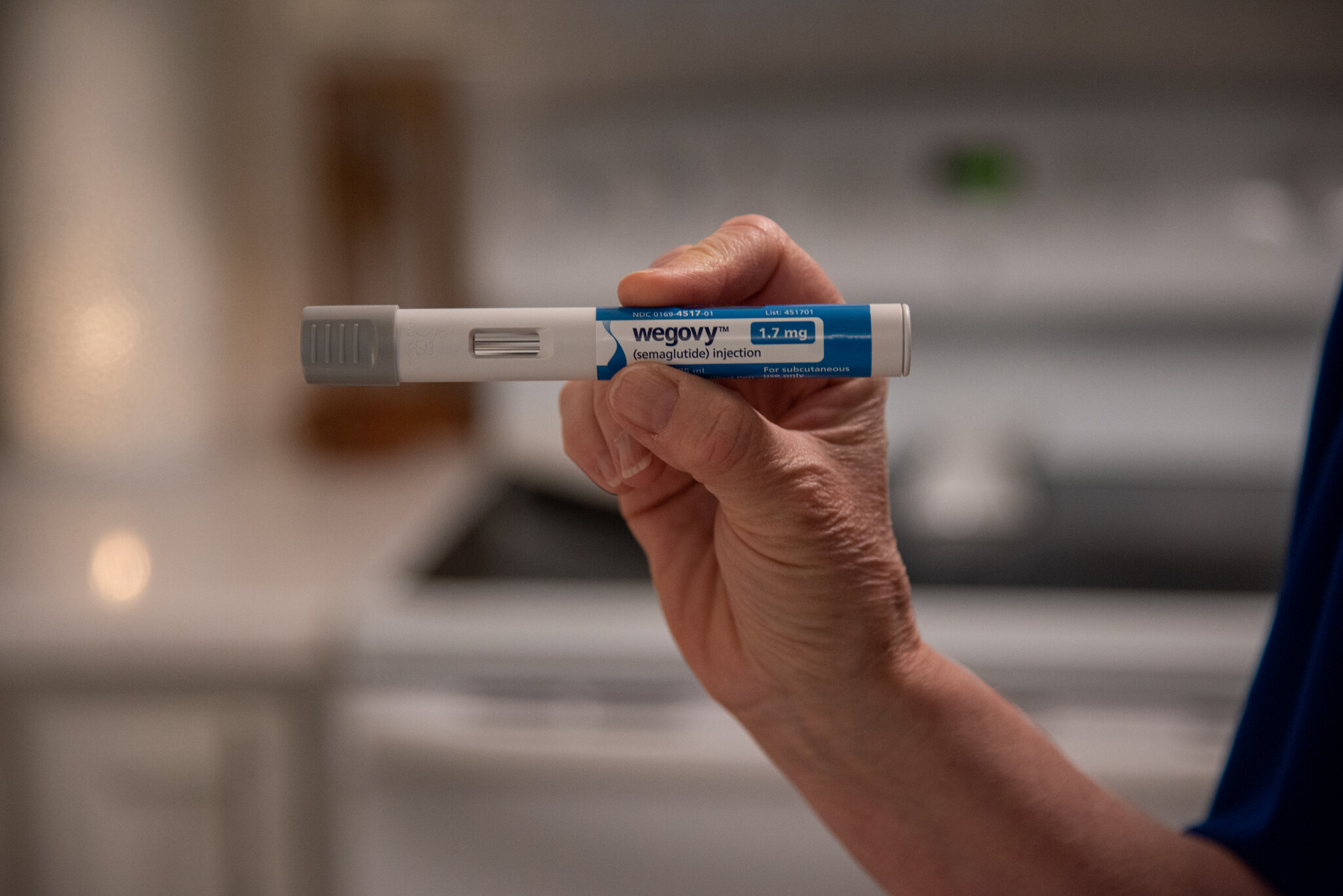
Millions of Americans who have successfully lost weight and improved their health with popular obesity drugs like Wegovy are now facing a new dilemma: What happens if they stop taking them?
Many are concerned about regaining weight and falling back into old habits, as clinical trials have shown that patients who pause these medications often regain most of the weight they had lost.
However, some are trying a self-managed approach to taper off the drugs and maintain their weight loss. This approach includes strategies like spacing out doses, taking the medication intermittently, or stopping and starting again as needed.
Donna Cooper, 62, of Front Royal, Virginia, who lost nearly 40 pounds in nine months using Wegovy alongside diet and exercise, sees the drug as a temporary aid. “To me, it’s a help, it’s an aid,” she said. “At some point, you have to come off of them. I don’t want to be on them forever.”
While more than 3 million prescriptions for these medications are dispensed each month in the U.S., many people do not continue taking them long-term. A study published in the journal Obesity found that only 40% of patients who filled a prescription for Wegovy in 2021 or 2022 were still taking it a year later.
Doctors emphasize that obesity is a chronic condition requiring ongoing management, similar to heart disease or high blood pressure. The new injection drugs work by mimicking hormones in the gut and brain to regulate appetite and fullness and were intended to be taken continuously.
Dr. Andres Acosta, an obesity researcher and medical adviser at the Mayo Clinic, emphasized that these drugs are not meant for intermittent use. “We are not an injection shop,” he said. “I don’t think they should be used in intermittent fashion. It’s not approved for that. They don’t work like that.”
Despite these recommendations, some patients who have achieved their health and weight loss goals with these drugs are looking for ways to reduce their dose or eventually stop taking them, according to Dr. Amy Rothberg, a University of Michigan endocrinologist. “Many of them want to step down or de-escalate their dose,” she said. “And they’re also wanting to ultimately discontinue the medication.”
Dr. Katherine Saunders, an obesity expert at Weill Cornell Medicine and co-founder of the obesity treatment company Intellihealth, noted that reasons for pausing obesity drugs can vary. Some patients dislike side effects like nausea and constipation, while others want to take a break for holidays, special occasions, or simply because they are unwilling to take weekly shots indefinitely.
One of Saunders’ patients, a 53-year-old man from New York, lost 70 pounds last year using Mounjaro. He expressed a desire to take “a breather” from the medication to observe how his body responds. Following Saunders’ advice, he has been spacing out his injections to every 10 days or two weeks instead of weekly since December.
Patients may also be forced to ration or discontinue doses due to the high cost of the drugs, ranging from $1,000 to $1,300 per month, and inconsistent insurance coverage. Some have had to stop because of the overwhelming demand for the drugs, leading to supply shortages.
However, hoping that the benefits of these drugs will persist after stopping them overlooks the fundamental biology of obesity. Obesity affects how the body processes and stores energy, leading to weight gain. These drugs alter this process, and when patients stop taking them, the disease often returns, sometimes more aggressively.
Many patients who stop taking the medications experience a resurgence of obesity symptoms, such as intrusive thoughts about food, increased hunger, and decreased feelings of fullness when eating.
Tara Rothenhoefer, 48, from Trinity, Florida, lost over 200 pounds after participating in a clinical trial for Mounjaro nearly four years ago. She now takes the lowest dose of the drug every four to eight weeks but becomes anxious when her weight fluctuates.
Some patients who stop and then restart these drugs find that they cannot tolerate them anymore, experiencing severe gastrointestinal side effects. Others find that the drugs are less effective when they resume them. However, there is no data on the long-term effects of intermittent use.
Donna Cooper, who has gone from a size 16 to a size 10 with the help of Wegovy, has heard about weight regain after stopping the drugs but hopes to be an exception. She is finishing her last box of Wegovy injections and plans to maintain her weight with a strict diet and exercise regimen.
“I just needed a crutch to get everything back in order,” said Cooper. “And I am excited to be done.”